Viral Vector Vaccine - 7 Facts You Might Not Know
Table of contents
ShowAmong the various vaccines available, viral vector vaccines are among the most innovative approaches. They use different viruses (viral vectors) that are able to deliver genetic material into the body, and can even enter cells to use their machinery to producing desired proteins, functioning as antigens that the immune system can react to.
This article will discuss several aspects of viral vector vaccines: We will uncover seven intriguing facts that shed light on this technology: From the ability to mimic infections to the challenges of storage and the diverse applications, these facts will not only expand your understanding of viral vector vaccines but also illuminate their role in shaping the future of vaccine development.
Fact 1: You might already have received a viral vector vaccine
In the global effort to combat the COVID-19 pandemic, a variety of vaccines have emerged as critical tools in the fight.
Unlike the RNA vaccines developed by Moderna and Pfizer-BioNTech, viral vector vaccines harness the power of viruses to deliver critical genetic material into our cells. Two notable examples of viral vector COVID-19 vaccines are those from AstraZeneca and Johnson & Johnson.
This type of vaccine uses a harmless adenovirus, modified to carry a piece of genetic code from the SARS-CoV-2 virus, that encodes for the spike protein. When administered, the immune system recognizes this spike protein as foreign, mounting a robust defense to generate immunity. This approach has earned both AstraZeneca and Johnson & Johnson vaccines Emergency Use Authorization (EUA) and widespread usage in many parts of the world.
Fact 2: There are two types of viral vector vaccines with several applications
The world of viral vector vaccines is a tapestry of diversity, offering a spectrum of types and applications with profound implications for preventive medicine and vaccination strategies. In general, two types of viral vector vaccines can be distinguished: While replicating viral vector vaccines use viruses that are capable of producing new viral particles after administration, non-replicating viral vector vaccines only replicate the vaccine antigen.
Examples of viral vector vaccines against COVID-19 include the Oxford-AstraZeneca vaccine, using a chimpanzee adenovirus as its vector, and the Janssen vaccine, which employs a human adenovirus. Both exemplify the ingenuity of viral vector-based vaccines, classified as recombinant, as they introduce genetic material from specific pathogens into the viral vector.
Beyond their COVID-19 applications, viral vector vaccines are promising tools in tackling outbreaks of diseases such as Zika or Ebola – in fact, the WHO was already positive about the safety of a viral vector vaccine candidate against the Ebola virus. This demonstrates the adaptability and vital role of viral vector technology not only in possible Ebola vaccines, but in infectious disease control generally. Moreover, these vaccines are intensely studied in the field of gene therapy, offering potential treatments for genetic disorders and various medical conditions.
1 2
Fact 3: Viral vector vaccines mimic infection
Viral vector vaccines, such as those based on adenoviruses, cleverly mimic a natural infection without causing disease. They introduce specific nucleic acid sequences from a virus's genome into host cells, triggering the immune system into action.
Immune cells recognize the foreign genetic material, kickstarting a response. In the case of COVID-19 vaccines, antigen-presenting cells display spike protein fragments, then alert B cells and T cells. B cells produce antibodies targeting the spike protein, while T cells help coordinate the response.
By training the immune system in this way, viral vector vaccines prepare it to effectively the actual virus effectively.
Fact 4: Side effects are rarely encountered
A notable aspect of viral vector vaccines is their favorable safety profile. The occurrence of serious side effects, including adverse events, is particularly rare with coronavirus vaccines.
The most common reported side effects are mild and transient, primarily localized to the injection site. These may include mild pain, redness, or swelling. In addition, individuals may experience fatigue, or headache – effects that may last for a few days.
It's important to note that these mild side effects are an indication of a strong immune response. They mean that the vaccine is actively engaging the immune system, a critical factor in providing protection against the target pathogen.
3
Fact 5: More than one virus is suitable for viral vector vaccine production
Viral vector vaccines are versatile and adaptable, using a variety of viruses as carriers for vaccine delivery. Among these, adenoviruses stand out as a commonly utilized vector. These adenovirus-based vaccines are engineered to deliver genetic material, often a portion of the target pathogen's genome, into host cells.
However, adenoviruses are only one of many potential viral vectors. Other viral vectors, such as vaccinia, are being explored for their suitability in vaccine production, gene therapy, and infectious disease control.
These vectors can be engineered to carry various genetic materials, allowing for tailored approaches to vaccine development. Additionally, some viral vector vaccines are produced using inactivated vectors, which enhances their safety and efficacy profiles.
The ability to use a variety of viruses as vectors enhances our ability to develop vaccines against a wide range of pathogens, underscoring the adaptability and potential of viral vector technology in the field of immunization.
Fact 6: Viral vector vaccine development can extend over years
Viral vector vaccine development is a meticulous and time-consuming process. It involves several critical stages that require rigorous evaluation, often taking years from design to approval.
The journey begins with vaccine design, which involves extensive research and preclinical studies. Scientists carefully design and evaluate vaccine components in the laboratory to ensure both safety and efficacy.
Clinical trials make up a significant portion of the timeline, and span multiple phases. These trials require thorough human testing to determine safety, optimal dosage and efficacy. They can last for several years and encompass a large number of participants.
Regulatory authorities such as the U.S. Food and Drug Administration (FDA) play a central role in evaluating the vaccine's safety and efficacy through a stringent review process.
Once a vaccine candidate is approved, the manufacturing process must be adapted and scaled up to bulk production. This can be another challenge in bringing a vaccine candidate to market, as the scale-up process can be costly. As a result, many manufacturers begin with scalable platforms in the first place, that allow them to more easily scale up vaccine production.
Fact 7: Viral vector vaccines should not be frozen multiple times
The efficacy of viral vector vaccines comes hand-in-hand with demanding storage requirements. These vaccines often require ultra-cold temperatures, plunging as low as -70°C (-94°F). Additionally, there are several aspects to be considered for viral vector vaccine storage, such as freezing rates or the fact that they should not be subjected to multiple freeze/thaw cycles, but rather a single one.
The Centers for Disease Control and Prevention (CDC) and healthcare providers play a critical role in maintaining vaccine efficacy through vigilant storage practices. Additionally, adapting vaccines to combat emerging variants further underscores the importance of flexibility and adaptability in the ongoing battle against infectious diseases.
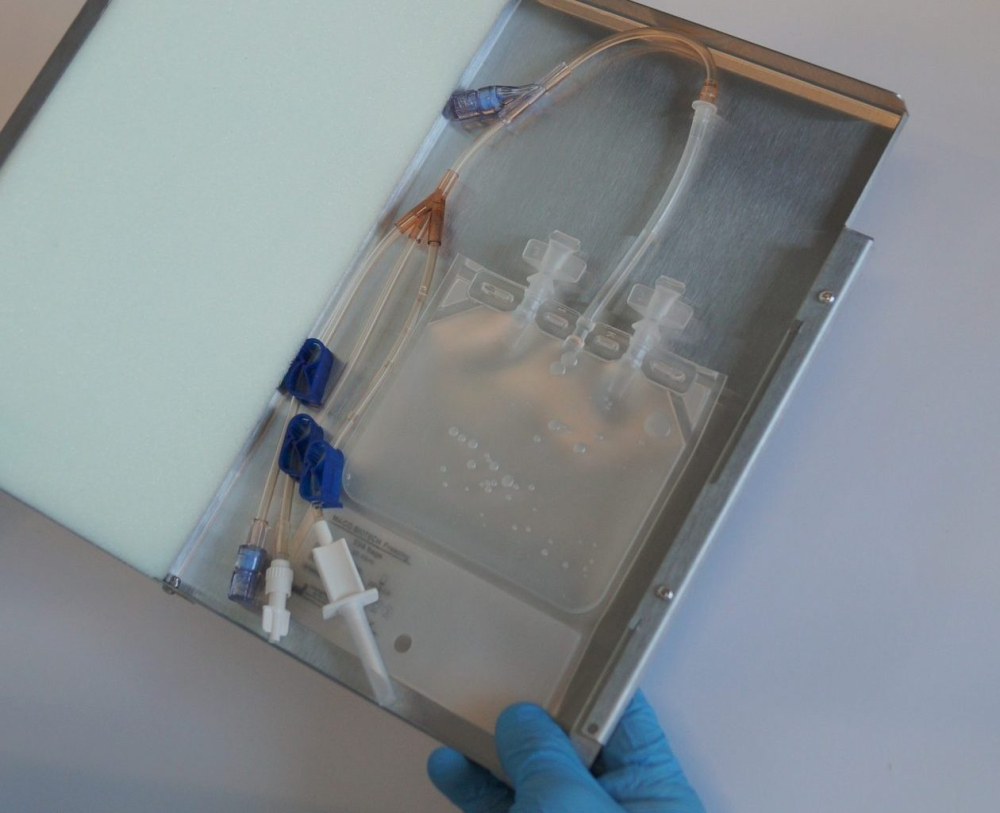
To ensure vaccine integrity, specialized freezers and precise transport protocols are essential. And as the volume of vaccines produced increases, so does the need for efficient solutions. Companies like Single Use Support specialize in streamlining the production of biopharmaceutical products, including ultra-low temperature vaccine storage.
Single Use Support has developed scalable fluid management and freezing platforms based on single-use technologies. Automated processes as well as fast and controlled freezing procedures are used to maintain the quality and efficacy of viral vector vaccines, while minimizing manufacturing costs and facilitating the production scale-up.

- , https://www.gavi.org/vaccineswork/what-are-viral-vector-based-vaccines-and-how-could-they-be-used-against-covid-19 , Published
- , https://www.who.int/groups/global-advisory-committee-on-vaccine-safety/topics/ebola-virus-vaccines , Published
- Side Effects of mRNA-Based and Viral Vector-Based COVID-19 Vaccines among German Healthcare Workers, http://dx.doi.org/10.3390/biology10080752, Published 2021-08-05