What is allogeneic?
Table of contents
ShowAllogeneic cell therapy is a type of stem cell therapy that uses stem cells from a donor to treat a recipient. When it comes to treating various medical conditions, including blood disorders and cancer, the field of regenerative medicine has introduced several innovative therapies, one of which is allogeneic cell therapy.
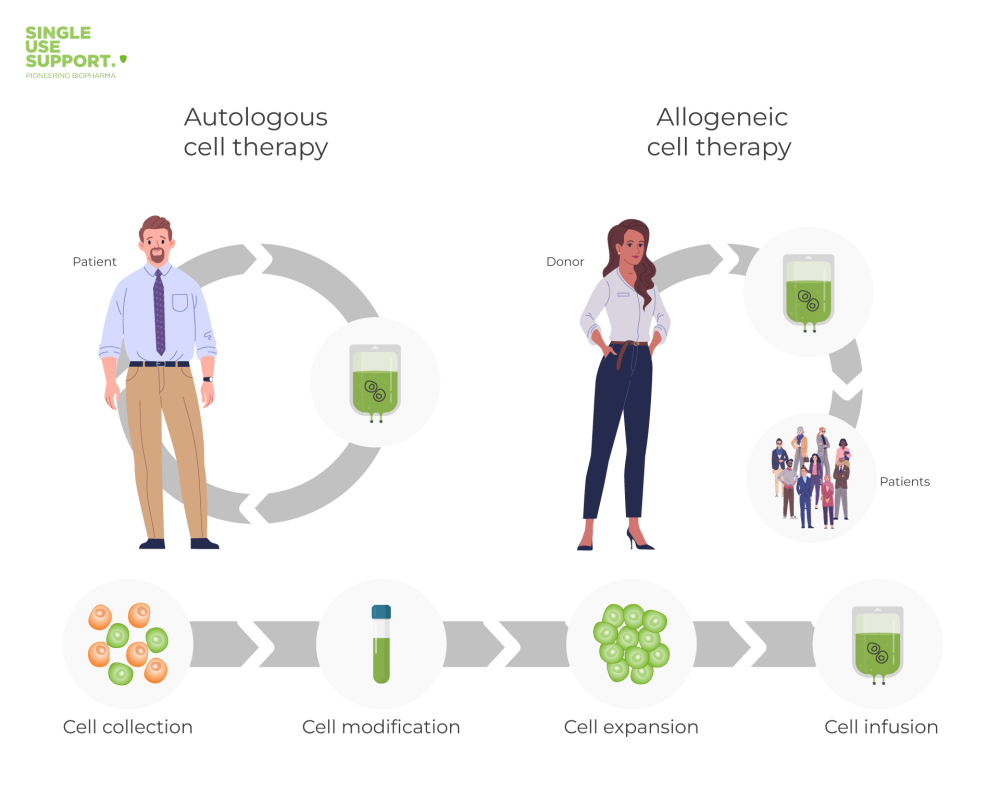
In this context, another approach often mentioned is autologous cell therapy. In general, allogeneic and autologous cell therapies differ in the type of cell donor: When performing autologous cell therapies, the cells do not come from donors, but from the patients themselves.
In this article, we will explore what allogeneic is, how it works, its further differences with autologous stem cell therapy, its fields of application, the procedure, and the various types of allogeneic stem cell transplants.
Allogeneic – The definition
Allogeneic refers to the transfer of cells, tissues, or organs from one individual of the same species to another. In the context of stem cell therapy, allogeneic cell therapy uses stem cells from a donor that are genetically different from the recipient's cells. These stem cells may come from a family member or an unrelated donor.1
How does an allogeneic stem cell transplant work?
An allogeneic stem cell transplant involves the infusion of healthy stem cells into a recipient's bloodstream. These stem cells will then migrate to the bone marrow and begin to produce new blood cells. This therapy is often used to treat various conditions, including leukemia, lymphoma, multiple myeloma, and myelodysplastic syndromes.
Before the allogeneic stem cell transplant, the recipient will undergo high doses of chemotherapy and/or radiation therapy. These treatments are aimed at destroying the recipient's cancer cells and suppressing their immune system to prevent rejection of the donor's stem cells. The donor stem cells are infused into the recipient's bloodstream via a catheter. The stem cells then travel to the bone marrow and begin producing new blood cells.
Allogeneic or autologous – here’s the difference
There are more than just terminological differences between “allogeneic” and “autologous”: Allogeneic stem cell therapy uses stem cells from a donor, whereas autologous stem cell therapy uses stem cells from the recipient's own body. With autologous stem cell therapy, the recipient undergoes a procedure to collect their own stem cells, which are then stored and later re-infused after high doses of chemotherapy and/or radiation therapy.
Read also: What is autologous?
One advantage of autologous stem cell therapy is that it eliminates the risk of graft-versus-host disease (GVHD) since the cells are genetically identical to the recipient's cells. However, allogeneic stem cell therapy is often preferred when the recipient does not have healthy stem cells or if the recipient has a high risk of relapse.2
Fields of application for allogeneic cell therapy
In the following, we will discuss two of the most important fields of application for allogeneic cell therapy.
Oncology
Allogeneic stem cell therapy is commonly used to treat various types of blood cancers, including leukemia, lymphoma, and multiple myeloma. This kind of cancer treatment aims to destroy the cancer cells and replace them with healthy stem cells.
Blood disorders
Allogeneic stem cell therapy is also used to treat certain blood disorders, including myelodysplastic syndromes and aplastic anemia. In these conditions, the bone marrow is unable to produce enough healthy blood cells, and allogeneic stem cell therapy can help restore blood counts.
Allogeneic cell therapy – the procedure
Allogeneic cell therapy is usually performed after a biopsy has determined that a patient is a candidate for the therapy. The allogeneic stem cell transplant procedure itself involves several steps, including:
- Preparative treatments such as chemotherapy and/or radiation therapy to destroy the recipient's cancer cells and suppress their immune system
- Infusion of donor stem cells via a catheter into the recipient's bloodstream
- Monitoring of the recipient's blood counts and immune system function to ensure engraftment of the donor's stem cells
- Management of potential side effects, including GVHD and infections
Preparative therapy is the use of high doses of chemotherapy and/or radiation therapy to eliminate cancer cells or suppress the immune system in the case of blood disorders. This helps to create a favorable environment for the donor stem cells to engraft and start producing new healthy blood cells.
The transplantation involves the infusion of donor stem cells into the patient's bloodstream via a catheter, often previously being stored in ultra-cold freezers to maximize their viability ex vivo. The stem cells then migrate to the bone marrow, where they begin to engraft and create new blood cells, including white blood cells, red blood cells, and platelets.
Engraftment is the process by which the donor stem cells settle into the bone marrow and begin to produce new blood cells. This process can take several weeks, and during this time, the patient may require blood transfusions and other supportive care.
Recovery involves monitoring the patient's blood counts and immune function and providing supportive care as needed. The patient may also need to take medications to prevent graft-versus-host disease (GVHD), a complication in which the donor immune cells attack the patient's tissues.
Suitable donors for allogeneic stem cell transplantation
A suitable donor for allogeneic stem cell transplantation is favorably a close genetic match to the patient to minimize the risk of GVHD and ensure engraftment. The ideal donor is often a family member, but if no suitable family member is available, the patient's medical team may turn to national donor registries to search for an unrelated donor.
The search for a matching donor involves testing for human leukocyte antigen (HLA) compatibility. HLA is a group of proteins found on the surface of cells that play a key role in the immune system's ability to distinguish self from non-self. The closer the match between the patient and donor's HLA, the lower the risk of GVHD and the higher the chances of successful engraftment.
Various types of allogeneic stem cell transplants
There are several different types of allogeneic stem cell transplants, which can be classified based on the type of donor, the source of stem cells, and the degree of matching between the donor and recipient. Here are the most common types:
- HLA-matched sibling transplant: In this type of transplant, the donor is a sibling who has a tissue type that closely matches the recipient's. This is considered the best type of transplant, as it has the highest success rate and the lowest risk of complications.3
- HLA-matched unrelated donor transplant: If a patient does not have a matching sibling, doctors can search for a matching donor in national or international registries. The donor can be from any ethnic group or country, but their HLA tissue type must be a close match to the recipient's. This type of transplant is associated with a higher risk of complications and a lower success rate compared to a sibling transplant.
- Haploidentical transplant: This type of transplant uses stem cells from a donor who is a half-match or partially matched relative, usually a parent, child, or sibling. It is a newer type of transplant, but it has shown promising results in recent years.
- Umbilical cord blood transplant: This type of transplant uses stem cells from the umbilical cord of a newborn baby. The advantage of this type of transplant is that the stem cells are readily available, and there is less need for a perfect match. However, the number of stem cells is limited, so this type of transplant is mostly used for children and young adults.
- T-cell depleted transplant: In this type of transplant, the stem cells are treated to remove the T-cells, which are responsible for graft-versus-host disease. This reduces the risk of GVHD, but it also increases the risk of infection and relapse.
- Reduced-intensity or non-myeloablative transplant: This type of transplant uses lower doses of chemotherapy and radiation therapy to prepare the patient for the transplant. This is a less toxic and less aggressive approach, which is suitable for older patients and those with other health problems.
Each type of transplant has its own advantages and disadvantages, and the choice of transplant depends on several factors, such as the patient's age, overall health, disease type and stage, and availability of a donor.3
Challenges for biopharma processing in allogeneic cell therapy
Despite the promising potential of allogeneic cell therapy, there are several challenges that the biopharma industry faces in processing and manufacturing them.
One of the major challenges is the ability to consistently produce high-quality cell products at scale. The complex and sensitive nature of cell therapies requires strict adherence to, e.g., freezing protocols, quality control measures, and environmental conditions to ensure reproducibility and consistency across multiple batches. This can be particularly challenging in allogeneic cell therapy, where cells from a donor must be processed and expanded to generate a sufficient number of cells for transplantation.
Another challenge is the need for specialized facilities and equipment to support the manufacturing process. These facilities must meet stringent regulatory requirements to ensure the safety and efficacy of the final product. Additionally, the machines used along the processing have to be suitable for the handling of minute units of biological material, which demands high levels of accuracy.
After being collected and filled into bioprocessing containers, allogeneic cell therapies are usually not immediately transplanted. Instead, they have to be frozen in order to prevent deterioration and allowing long-term storage. Therefore, specialized freeze/thaw units are required that are cost-effective and allow for fast and controlled freezing, preventing cryoconcentration and other effects that might impact quality and viability.
Nevertheless, allogeneic stem cell therapy offers several unique advantages, making it only logical for the biopharma industry to face related challenges with innovative technologies.

Conclusion – why allogeneic stem cell therapy is essential
Allogeneic cell therapy, including hematopoietic stem cell transplantation and allogeneic bone marrow transplant, is a viable treatment option for patients with certain types of blood cancer, myelodysplastic syndromes, and aplastic anemia. Clinical trials and platforms like the National Marrow Donor Program have made it possible for more patients to find a matching donor and receive a blood stem cell transplant.
Research in the field of cell therapies is pushing the potentials of allogeneic stem cell transplantation even further, which is why healthcare providers, researchers and manufacturers are in need of novel techniques as well as highly specialized equipment.
Therefore, Single Use Support has developed a product line-up that accompanies cell therapies across large parts of their mission: With single-use bioprocess containers, a plate freezing platform, ultra-cold storage solutions and devices for automated filling of even extremely small volumes, Single Use Support is determined to contribute to even more groundbreaking achievements in the field of cell therapy.
- National Cancer Institute / Dictionary of Cancer Terms: "allogeneic", https://www.cancer.gov/publications/dictionaries/cancer-terms/def/allogenic, Published
- Selection of Autologous or Allogeneic Transplantation, https://www.ncbi.nlm.nih.gov/books/NBK12844/, Published 2003
- Which is better, HLA-matched sibling or haploidentical transplantation?, http://dx.doi.org/10.1038/s41423-021-00640-9, Published 2021-04-20









